Outer segment formation of transplanted photoreceptor precursor cells.
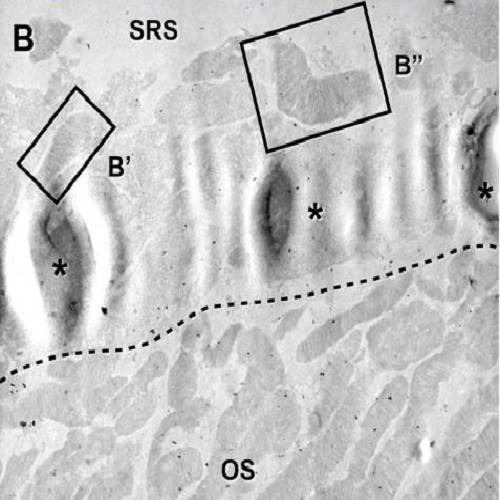
Transplantation of photoreceptor precursor cells (PPCs) into the retina represents a promising treatment for cell replacement in blinding diseases characterized by photoreceptor loss. In preclinical studies, we and others demonstrated that grafted PPCs integrate into the host outer nuclear layer (ONL) and develop into mature photoreceptors. However, a key feature of light detecting photoreceptors, the outer segment (OS) with natively aligned disc membrane staples, has not been studied in detail following transplantation. Therefore, we used as donor cells PPCs isolated from neonatal double transgenic reporter mice in which OSs are selectively labeled by green fluorescent protein while cell bodies are highlighted by red fluorescent protein. PPCs were enriched using CD73-based magnetic associated cell sorting and subsequently transplanted into either adult wild-type or a model of autosomal-dominant retinal degeneration mice. Three weeks post-transplantation, donor photoreceptors were identified based on fluorescent-reporter expression and OS formation was monitored at light and electron microscopy levels. Donor cells that properly integrated into the host wild-type retina developed OSs with the formation of a connecting cilium and well-aligned disc membrane staples similar to the surrounding native cells of the host. Surprisingly, the majority of not-integrated PPCs that remained in the sub-retinal space also generated native-like OSs in wild-type mice and those affected by retinal degeneration. Moreover, they showed an improved photoreceptor maturation and OS formation by comparison to donor cells located on the vitreous side suggesting that environmental cues influence the PPC differentiation and maturation. We conclude that transplanted PPCs, whether integrated or not into the host ONL, are able to generate the cellular structure for effective light detection, a phenomenon observed in wild-type as well as in degenerated retinas. Given that patients suffering from retinitis pigmentosa lose almost all photoreceptors, our findings are of utmost importance for the development of cell-based therapies.
- PLoS ONE 2012 Sep 28;7(9):e46305
- 2012
- Cell Biology
- 23029471
- PubMed
Enabled by:
