Hematopoietic hypoxia-inducible factor 2α deficiency ameliorates pathological retinal neovascularization via modulation of endothelial cell apoptosis.
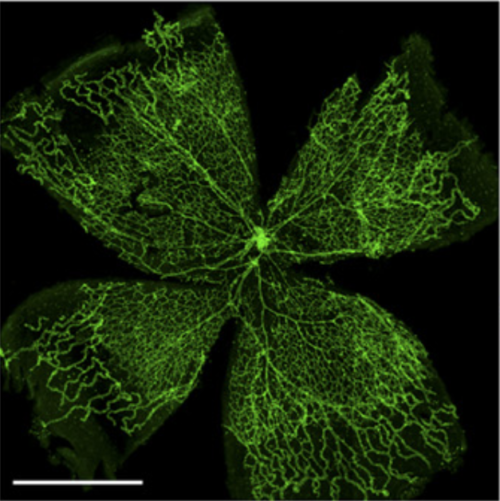
A hallmark of proliferative retinopathies, such as retinopathy of prematurity (ROP), is a pathological neovascularization orchestrated by hypoxia and the resulting hypoxia-inducible factor (HIF)-dependent response. We studied the role of Hif2α in hematopoietic cells for pathological retina neovascularization in the murine model of ROP, the oxygen-induced retinopathy (OIR) model. Hematopoietic-specific deficiency of Hif2α ameliorated pathological neovascularization in the OIR model, which was accompanied by enhanced endothelial cell apoptosis. That latter finding was associated with up-regulation of the apoptosis-inducer FasL in Hif2α-deficient microglia. Consistently, pharmacological inhibition of the FasL reversed the reduced pathological neovascularization from hematopoietic-specific Hif2α deficiency. Our study found that the hematopoietic cell Hif2α contributes to pathological retina angiogenesis. Our findings not only provide novel insights regarding the complex interplay between immune cells and endothelial cells in hypoxia-driven retina neovascularization but also may have therapeutic implications for proliferative retinopathies.-Korovina, I., Neuwirth, A., Sprott, D., Weber, S., Sardar Pasha, S. P. B., Gercken, B., Breier, G., El-Armouche, A., Deussen, A., Karl, M. O., Wielockx, B., Chavakis, T., Klotzsche-von Ameln, A. Hematopoietic hypoxia-inducible factor 2α deficiency ameliorates pathological retinal neovascularization via modulation of endothelial cell apoptosis.
- FASEB J. 2019 Feb;33(2):1758-1770
- 2019
- Medical Biology
- 30156910
- PubMed
Enabled by:
