Modelling pancreatic β-cell inflammation in zebrafish identifies the natural product wedelolactone for human islet protection.
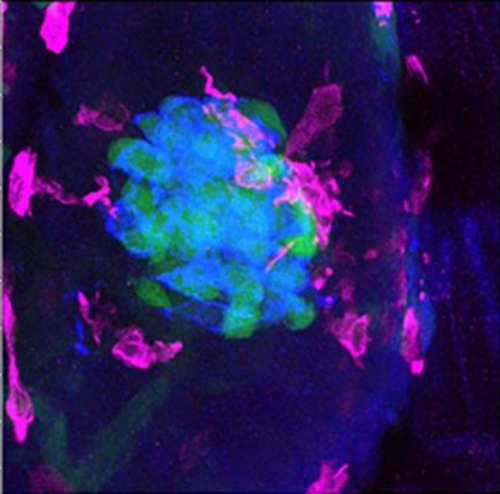
Islet inflammation and cytokine production are implicated in pancreatic β-cell dysfunction and diabetes pathogenesis. However, we lack therapeutics to protect the insulin-producing β-cells from inflammatory damage. Closing this clinical gap requires the establishment of new disease models of islet inflammation to facilitate screening efforts aimed at identifying new protective agents. Here, we have developed a genetic model of Interleukin-1β (Il-1β)-driven islet inflammation in zebrafish, a vertebrate that allows for non-invasive imaging of β-cells and in vivo drug discovery. Live imaging of immune cells and β-cells in our model revealed dynamic migration, increased visitation and prolonged macrophage retention in the islet, together with robust activation of NF-κB signalling in β-cells. We find that Il-1β-mediated inflammation does not cause β-cell destruction but, rather, it impairs β-cell function and identity. In vivo, β-cells exhibit impaired glucose-stimulated calcium influx and reduced expression of genes involved in function and maturity. These defects are accompanied by α-cell expansion, glucose intolerance and hyperglycemia following a glucose challenge. Notably, we show that a medicinal plant derivative (wedelolactone) is capable of reducing the immune-cell infiltration while also ameliorating the hyperglycemic phenotype of our model. Importantly, these anti-diabetic properties in zebrafish are predictive of wedelolactone's efficacy in protecting rodent and human islets from cytokine-induced apoptosis. In summary, this new zebrafish model of diabetes opens a window to study the interactions between immune and β-cells in vivo, while also allowing the identification of therapeutic agents for protecting β-cells from inflammation.
Back to list